Understanding the Different Types of Stroke
Welcome to our comprehensive guide on understanding the different types of stroke. In this post, we will explore the various types of strokes, their causes, symptoms, and treatment options.
A stroke occurs when the blood supply to the brain becomes interrupted, leading to damaged or destroyed brain cells. It is important to understand that not all strokes are the same. Knowing the differences between strokes can impact treatment and recovery significantly.
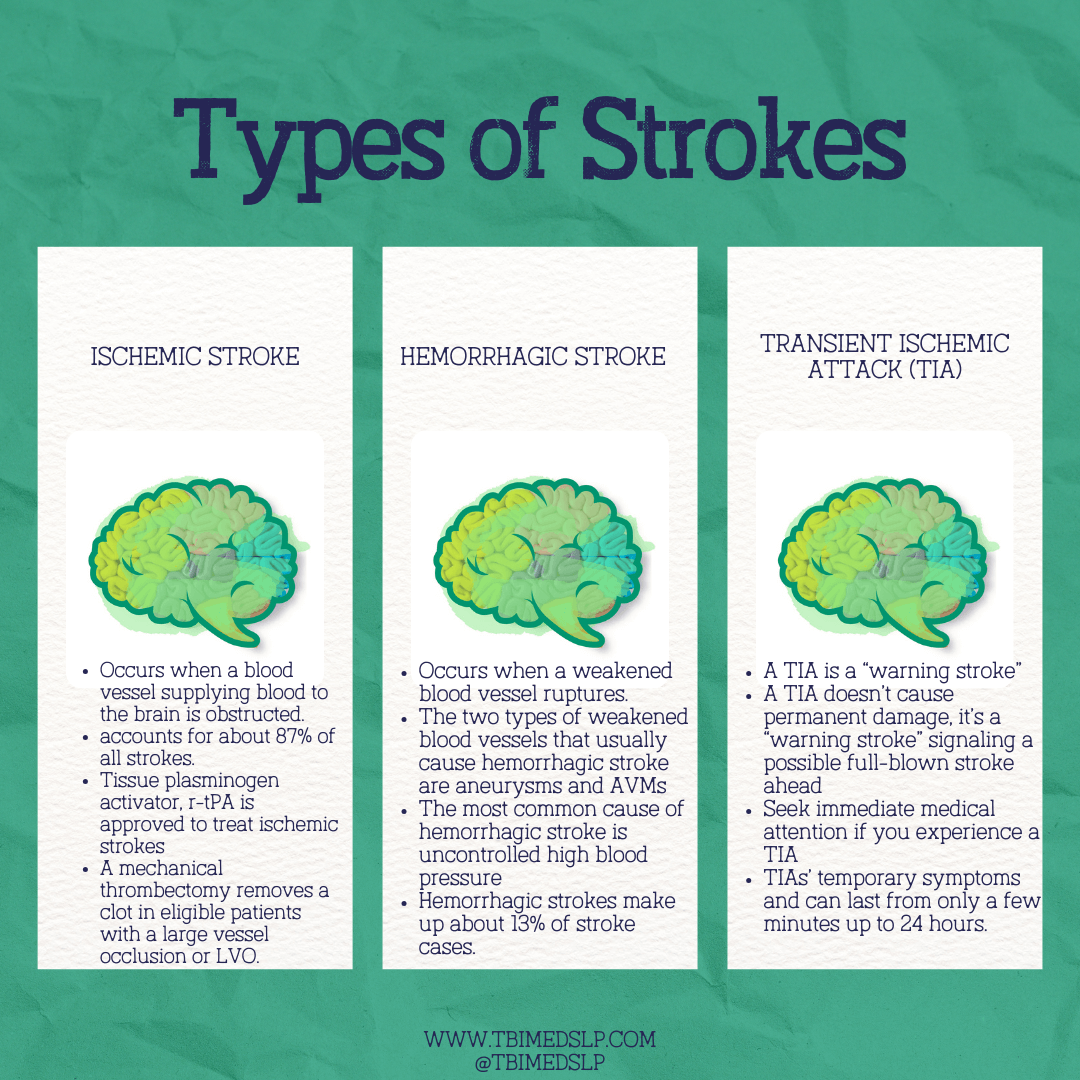
Ischemic stroke, hemorrhagic stroke, and transient ischemic attack (TIA) are the three main types of strokes. An ischemic stroke happens from a blood clot blocking an artery in the brain. A hemorrhagic stroke is the result of a ruptured blood vessel. A TIA, also known as a mini-stroke, is a temporary interruption of blood flow to the brain.
By understanding the specific characteristics and risk factors associated with each type of stroke, individuals can take preventative measures and seek appropriate medical attention. Awareness and education are key in minimizing the devastating impact of strokes.
Ischemic Strokes: Causes, Symptoms, and Treatment
Ischemic strokes are the most common type of stroke. They account for approximately 87% of all strokes. These strokes occur when a blood clot blocks an artery in the brain, cutting off the blood supply and oxygen to a particular area of the brain.
There are two main types of ischemic stroke: thrombotic stroke and embolic stroke. A thrombotic stroke occurs when a blood clot forms within one of the arteries leading to the brain. This is often a result of atherosclerosis, a condition where fatty deposits build up in the arteries, causing them to narrow and become blocked. An embolic stroke occurs when a blood clot or plaque fragment forms elsewhere in the body, such as the heart or neck, and travels to the brain, blocking a blood vessel.
The symptoms of an ischemic stroke can vary depending on the area of the brain affected.
Common symptoms include:
sudden weakness or numbness on one side of the body
difficulty speaking or understanding speech
vision problems
severe headache
dizziness
If you or someone around you experiences these symptoms, call 911 immediately.
Treatment for ischemic stroke aims to restore blood flow to the affected area of the brain as quickly as possible. One common treatment option is the administration of clot-busting medications, such as tissue plasminogen activator (tPA), which can dissolve the blood clot and restore blood flow.
In some cases, medical procedures may be necessary to physically remove the clot, such as mechanical thrombectomy.
Hemorrhagic Strokes: Causes, Symptoms, and Treatment
Hemorrhagic strokes happen when a blood vessel in the brain ruptures. This leads to bleeding within or around the brain. This type of stroke accounts for approximately 13% of all strokes.
It is often more severe and life-threatening than ischemic strokes.
There are two main types of hemorrhagic stroke: intracerebral hemorrhage and subarachnoid hemorrhage. An intracerebral hemorrhage occurs when a blood vessel within the brain bursts, causing bleeding and damage to the surrounding brain tissue. Subarachnoid hemorrhage, is a rupture of a blood vessel on the surface of the brain, leading to bleeding in the space between the brain and the skull.
The symptoms of a hemorrhagic stroke can be similar to those of an ischemic stroke. Hemorrhagic stroke symptoms may also include a sudden and severe headache, nausea, vomiting, seizures, and loss of consciousness. It is crucial to seek immediate medical attention if you suspect a hemorrhagic stroke.
Treatment for hemorrhagic stroke focuses on controlling bleeding, reducing pressure on the brain, and preventing further damage. In some cases, surgery may be necessary to repair the ruptured blood vessel or remove accumulated blood. Medications to control blood pressure and prevent seizures may also be prescribed.
Transient Ischemic Attacks (TIAs): Causes, Symptoms, and Treatment
Transient ischemic attacks, often referred to as mini-strokes, are temporary interruptions of blood flow to the brain. While TIAs generally do not cause permanent damage, they are significant warning signs of an increased risk of a full-blown stroke.
TIAs are a temporary blockage or reduction of blood flow to the brain, usually due to a blood clot. The symptoms of a TIA are similar to those of an ischemic stroke but often resolve within a few minutes to a few hours. These symptoms may include sudden weakness or numbness on one side of the body, difficulty speaking or understanding speech, vision problems, and dizziness.
It is crucial not to ignore the symptoms of a TIA, as they can provide valuable insights into the underlying causes and risk factors for stroke. Seeking medical attention after experiencing a TIA can help identify and manage these risk factors, potentially preventing a future stroke.
Treatment for TIAs focuses on addressing the underlying causes and reducing the risk of a future stroke. Lifestyle changes, such as quitting smoking, managing high blood pressure, and controlling diabetes, are often recommended. Medications to prevent blood clots, lower cholesterol levels, and manage other risk factors may also be prescribed.
Risk Factors for Strokes
Knowing the risk factors associated with strokes is essential for prevention and early intervention. While some risk factors cannot be changed, such as age, family history, and race. Other risk factors can be managed or modified to reduce the risk of stroke.
High blood pressure is the leading risk factor for strokes. Monitoring blood pressure regularly and taking steps to control it is essential. Other lifestyle changes such as maintaining a healthy diet, exercising regularly, and taking prescribed medications if necessary are preventative stroke steps. Other modifiable risk factors include smoking, obesity, high cholesterol levels, diabetes, excessive alcohol consumption, and physical inactivity. Talk with your healthcare provider about managing these risk factors to decrease your risk of stroke.
Certain medical conditions, such as atrial fibrillation (an irregular heartbeat), carotid artery disease, and sickle cell disease, can also increase the risk of strokes. It is important to work closely with healthcare professionals to manage these conditions and minimize the associated risks.
Furthermore, lifestyle factors, such as poor diet and lack of physical activity, can contribute to an increased risk of strokes. Adopting a healthy lifestyle, including a balanced diet, regular exercise, and stress management, can reduce the risk of strokes.
Recognizing the Signs and Symptoms of a Stroke
Recognizing the signs and symptoms of a stroke is crucial for immediate medical intervention. Early treatment can greatly improve outcomes. The acronym BE FAST can help individuals identify the signs of a stroke:
Balance: You may feel a lack of balance, difficulty when walking, or dizziness.
Eyes: You may have blurry or double vision. You may also notice a lack of vision in one eye or loss of vision in one visual field.
Face drooping: One side of the face may droop or feel numb. Ask the person to smile to check for any asymmetry.
Arm weakness: One arm may feel weak or numb. Ask the person to raise both arms to check for any arm drift.
Speech difficulty: Speech may be slurred or difficult to understand. Ask the person to repeat a simple sentence to check for any speech abnormalities.
Time to call emergency services: If any of the above symptoms are present, it is essential to call emergency services immediately.
In addition to the BE FAST acronym, other common symptoms of a stroke include sudden severe headache, confusion, trouble seeing in one or both eyes, difficulty walking, and dizziness.
Remember, every minute counts when it comes to stroke treatment. Do not hesitate to call emergency services if you suspect a stroke.
Diagnosing Strokes: Tests and Procedures
Prompt and accurate diagnosis is critical for effective stroke treatment. When a stroke is suspected, healthcare professionals will conduct a series of tests and procedures to confirm the diagnosis and determine the type of stroke.
Physical examinations, including assessing neurological functions, can provide insights into a possible stroke. Imaging tests, such as computed tomography (CT) scans and magnetic resonance imaging (MRI), are used to visualize the brain and identify any abnormalities or signs of stroke.
Blood tests may be performed to evaluate blood clotting factors, cholesterol levels, and other potential causes of stroke. Electrocardiograms (ECGs) may be used to detect irregular heartbeat patterns that can increase the risk of stroke.
Speed and accuracy in diagnosis are vital to determine the appropriate treatment plan. This is important so that healthcare professionals can act quickly to minimize brain damage and maximize recovery potential.
Treatment Options for Strokes
Treatment for strokes depends on the type, severity, and timing of the stroke. The primary goals of treatment are to restore blood flow to the brain, prevent further damage, and support recovery.
For ischemic strokes, the administration of clot-busting medications, such as tissue plasminogen activator (tPA), is a common treatment option. These medications work by dissolving blood clots and restoring blood flow to the affected area of the brain. Mechanical thrombectomy is a procedure to physically remove the clot. It may also be considered in certain cases.
In cases of hemorrhagic strokes, the focus is on controlling bleeding, reducing pressure on the brain, and preventing further damage. Surgery may be necessary to repair blood vessels, remove accumulated blood, or relieve pressure. Medications to manage blood pressure, prevent seizures, and control other risk factors may also be prescribed.
Rehabilitation and Recovery after a Stroke
Rehabilitation plays a large role in stroke recovery. Rehab helps individuals regain lost abilities, learn new skills, and maximize independence. The specific rehabilitation program will depend on the individual's needs and the areas of the body or functions affected by the stroke.
Physical therapy aims to improve strength, coordination, and mobility. Occupational therapy focuses on enhancing the ability to perform daily activities, such as dressing, eating, and bathing. Speech therapy helps individuals regain or improve their communication, cognitive, and swallowing abilities. Psychological support is essential to address emotional and cognitive challenges post-stroke.
The duration and intensity of rehabilitation will vary depending on the individual and the extent of the stroke. Rehabilitation is often a long-term process that requires patience, perseverance, and a multidisciplinary approach. It involves healthcare professionals, caregivers, and the individual themselves.
Importance of Stroke Prevention and Awareness
Understanding the different types of stroke is crucial for prevention, early intervention, and effective treatment. Ischemic strokes, hemorrhagic strokes, and transient ischemic attacks (TIAs) each have distinct causes, symptoms, and treatment options. Recognizing the signs of a stroke and seeking immediate medical attention can significantly improve outcomes.
Risk factors for strokes, such as high blood pressure, smoking, obesity, and certain medical conditions, should be actively managed to reduce the risk. Lifestyle modifications, including a healthy diet, regular exercise, and stress management, can also play a significant role in stroke prevention.
Early diagnosis and appropriate treatment are essential for minimizing brain damage and optimizing recovery potential. Rehabilitation and support programs are vital for individuals to regain lost abilities and improve their quality of life post-stroke.
By increasing stroke prevention efforts, raising awareness, and promoting early intervention, we can reduce the devastating impact of strokes and protect our brain health. Stay informed, take action, and prioritize your well-being.
This blog post is for educational purposes and does not serve a medical advice or substitute recommendations of a healthcare provider